More Information
Submitted: November 28, 2024 | Approved: December 13, 2024 | Published: December 16, 2024
How to cite this article: Hugues JCO. Organizational and Human Factors in Dentistry: A Macroergonomic Approach to Maximize Dental Practice Performance and Minimize Burnout and Psychophysical Stress. J Clin Adv Dent. 2024; 8(1): 047-051. Available from: https://dx.doi.org/10.29328/journal.jcad.1001046
DOI: 10.29328/journal.jcad.1001046
Copyright License: © 2024 Hugues JCO. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Organizational and Human Factors in Dentistry: A Macroergonomic Approach to Maximize Dental Practice Performance and Minimize Burnout and Psychophysical Stress
Juan Carlos Ortiz Hugues*
Academy of Microscope Enhanced Dentistry (AMED), USA
*Address for Correspondence: Juan Carlos Ortiz Hugues, DDS CEAS II AEP, Academy of Microscope Enhanced Dentistry (AMED), USA, Email: [email protected]
The psychophysical impact of a high-complexity environment such as the dental office is not a novelty. This article outlines the organizational and human factors that impact the overall health of dentists, assistants, hygienists, and administrative staff. A careless organizational and human factors approach cannot only function as a stress and error trigger but also affect the highly precise requirements of dentistry and task performance in the daily demands of the office.
Ergonomics and human factors principles guidelines should be structured and taught from the basics in dental schools and supported by prevention programs and interventions in the dental professional field, as in other industries, to promote safety, health, and efficiency within the integration of humans, systems, and environments.
Usually, the main focus of dentistry research is the physical aspect of the job; the high rates of musculoskeletal disorders are a real problem, but the cognitive-organizational element of the job is not a minimal issue, which highly contributes to physical-emotional exhaustion in the work environment.
A fatigued mind impacts the physical aspect of the job, and physical fatigue impacts the mental aspect of the job. This dual effect in a job that requires dealing with anxiety and fear patients, administrative situations in the office, financial aspects, and technical and skill aspects from the dentist, among other requirements, makes dentistry a unique profession.
This article addresses the components of the factors that promote cognitive depletion in our field and provides simple tips on controlling them to avoid burnout among dentists. It highlights the importance of awareness of how we manage the organization in the office and the effect on human behavior and performance. It wants to bring to light a common problem for dental practitioners and the workforce to prevent health and performance decrease.
Dental professionals face unique challenges due to the high levels of responsibility, work pressure, and complex decision-making inherent in the field. Factors such as demotivation, time constraints, work-home stress, and team dynamics can either enhance workplace harmony or lead to cognitive strain and burnout for dental practitioners. Analyzing and managing both organizational and human factors—through frameworks commonly applied in high-stakes industries like aviation—can help reduce errors, improve performance, and create a safer, more productive practice environment [1].
Organizational factors and physical fatigue
Organizational factors and work practice behaviors require a comprehensive understanding of workplace dynamics and a deep analysis of how organizations function in the dental office and how they affect it. The dental office’s organizational aspect is affected by the environment in which it operates and can affect the efficiency, motivation, and performance of the people working in an environment of high demand for quality and precision.
While physical fatigue in dental practice is well-documented in ergonomic studies, the cognitive challenges faced by dental professionals also warrant careful attention [2]. The concept of human factors has been extensively studied in other fields, emphasizing error reduction and enhanced decision-making under pressure. For instance, aviation emphasizes critical decision-making processes and error minimization techniques, which, if applied to dentistry, can improve workflow and help prevent errors that may impact patient safety.
Dentistry demands rapid, continuous decision-making, particularly in high-stakes situations involving patient expectations, systemic conditions, operator expertise, and visual and cognitive demands. When combined with high levels of responsibility, these factors can profoundly impact both the outcomes of dental treatments and the cognitive resilience of the practitioner. Awareness of these cognitive demands allows for the identification of potential risks and opportunities to enhance decision-making within dental practices [3-5].
Human factors impacting cognitive load and performance
Dental practitioners frequently encounter unavoidable errors, whether from cognitive slips, knowledge gaps, or procedural complacency. These mistakes may arise from action or thought processing errors, insufficient knowledge, or the habitual repetition of tasks. Understanding the cognitive demands and potential errors within a dental setting can provide a roadmap for improvement.
Being able to identify capabilities, skills, attitudes, aptitudes, and continuous training must be part of the organizational logistics of each dental office to place people in positions where they can perform better and offer more predictable results.
Key cognitive factors to control in dental practice
1. Social psychology: Focusing on the work environment and the ownership- the workforce’s shared culture, values, and open communication can be the cornerstone of proper workflow and quality outcomes. According to social psychologists, creating an environment in the workplace that allows for the free flow of exchanging ideas, expertise, training, and social support will increase employees’ happiness and productivity and make them more likely to remain in their jobs [6].
Some of the factors to address are as follows [7,8]:
- Level of responsibility: Having clear responsibilities makes the operator and staff accountable for their respective tasks; it is essential to understand the work, the sense of accomplishment, and the employee's motivation.
- Motivation and demotivation: Motivation is a fundamental aspect of the job; working on our skills and our strengths in a positive working environment is essential to achieving better performance and high motivation.
- Peer pressure: Peer pressure can propitiate positive or negative stress, depending on personality. Clear and open communication and realistic goals between management, the dentist, and the staff or between peers can trigger excellent clinical outcomes with less stress.
- Communication between team members: Using guidelines, standard procedures, and communication within a detailed working system creates efficiency in the environment.
Incorporating tools like Lean Six Sigma can improve workflow by enhancing communication, training, and overall job satisfaction, helping to create an accountable, performance-driven culture. Techniques such as scheduled meditation, stretching, and work-life balance strategies can mitigate mental fatigue. Utilizing checklists and models like James Reason’s Swiss Cheese Model helps preemptively address potential errors, identify points of failure, and establish error-mitigation strategies [9-11].
2. Performance-affecting factors: High performance in a high-demand precision task profession and patient service management is fundamental to operating with excellence. Some of the factors affecting performance that need to be addressed and controlled are:
- Physical fitness: Poor stamina, postural muscle weakness, sedentarism, alcoholism, and smoking, among others, are risk factors for musculoskeletal disorders development. Physical fitness can improve job performance, reduce errors, and enhance decision-making skills [12].
- Time pressure and deadlines: It is well documented that time pressure affects the human body with strain, exhaustion, work engagement, and self-esteem. Schedule management must be realistic with the procedural times with patients and be strategic in the agenda organization [13].
- Home and work stress: High stress levels trigger multiple diseases; a combination of stress in the office and at home represents a source of demotivation, exhaustion, anxiety, fatigue, and lack of purpose for working at the maximum level [14].
- Workload and distraction management: Mental and physical workloads have been associated with increased muscle activity, spinal loads, and reports of discomfort [15].
Stressors such as obesity, lack of sleep, substance use, and inadequate work-life balance can decrease the cognitive and physical capabilities of dental practitioners. Many dental clinics operate under high time demands and workload pressures, often without structured time management strategies, which exacerbates stress and reduces performance [16,17].
Developing a well-organized system for scheduling, case selection, and staff rotation, coupled with continuous professional education, can help dental practices achieve optimal efficiency and reduce cognitive strain [18,19].
3. Situational awareness: Our ability to focus on the task at hand can sometimes be compromised by our situations, affecting the final results and the risk of accidents and errors [20].
Some of the factors to be aware of during procedural tasks;
- Awareness of time (Avoid time pressure)
- Awareness of surroundings (Avoiding distractions from the task)
- Team roles and dynamics (Define the roles depending on training, capabilities, and skills)
- Risk management (Clear guidelines)
Time awareness, task organization, and proper arrangement of workspace items based on efficient horizontal reaching areas for item/equipment placement can reduce unnecessary physical strain, interruptions, efficiency, and workflow and allow dentists to focus on critical tasks (Figure 1).
Figure 1: (a-c): Operatory Equipment, and Items Pre-Organization for Efficient Dentistry. (Images provided and owned by the author).
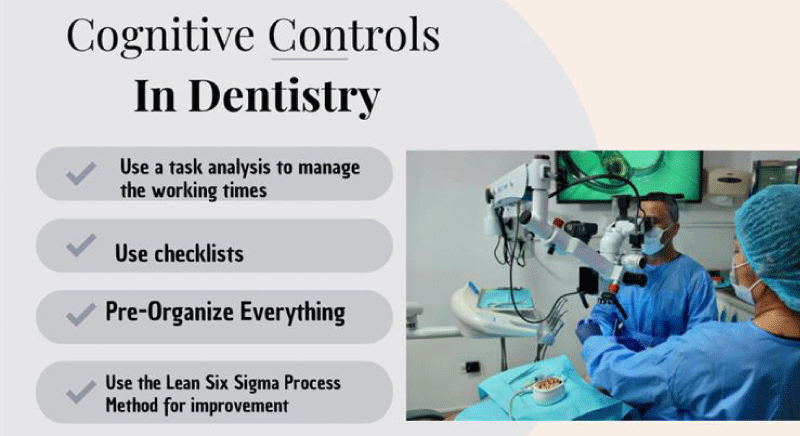
Using visual checklists, procedural clear, simplified guidelines, timers for break cycles, role definition, and task completion analysis promotes situational awareness, efficiency, uninterrupted workflow, motion controls, strategic pre-organization items, and time management control, minimizing the risk of errors and complacency in routine procedures [21] (Figure 2).
Figure 2: Tips for effective cognitive controls in dentistry. (Image provided and owned by the author).
4. Task complexity and repetition: The task complexity and the above-mentioned factors should be controlled to minimize physical and psychological constraints in dentistry;
- Physical strain from high-load tasks
- Cognitive demands of complex procedures
- Monotony from repetitive tasks
Traditional dentistry performed with standard magnification tools or the naked eye often leads to poor ergonomics, which may result in physical strain. The dental microscope, when used correctly, can improve posture, reduce fatigue, and enhance precision by allowing multiple levels of magnification [22].
Analyzing each dental task for its complexity and organizing patient treatment times accordingly can significantly reduce time pressures and improve cognitive efficiency [23]. For example, more complex procedures, such as molar endodontics or multi-tooth crowns, should be scheduled with adequate time and appropriate tools. Documenting approximate service times for each type of procedure can aid in managing time effectively, leading to smoother workflow and enhanced performance [24,25].
Adequate training for the assistant, considering ergonomic principles of work techniques, economy of movement, neutral posture, positioning and acquisition of a chair, and furniture with ergonomic design are investments that optimize and enhance the work workflow with the dentist and minimize mental and physical stress to the operator [26].
Burnout in Dentistry: Prevention and management
Burnout, a condition characterized by mental, emotional, and physical exhaustion, is common in healthcare. Symptoms include fatigue, negativity, mental disengagement, and reduced efficiency. Studies show that burnout affects a significant proportion of healthcare workers, including 57% of internal medicine students and 38% of cardiologists [27,28]. Among dentists, one in ten reports symptoms of burnout, primarily emotional exhaustion and depersonalization [29,30].
High workload, stress, demanding work conditions, and patient expectations contribute to absenteeism, lower productivity, and decreased job satisfaction. Managing workload effectively and promoting a balanced work-life approach is essential to combat burnout. Techniques like mindfulness, communication improvement, and dedicated relaxation time help alleviate workplace stress [31,32].
The “3 Rs” approach—Relax, Reflect, and Regroup—offers a structured method for preventing burnout. Regular relaxation alleviates exhaustion, reflection helps identify potential improvements, and regrouping encourages strategy development for addressing challenges [33].
Tips for burnout control in dentistry:
- Look for Colleagues' Support System when having feelings of anxiety, dissatisfaction, and mental exhaustion.
- Drop, Delegate, and Redesign; shift for better work practices, support for the staff, and redesigning tasks, procedures, and working methodologies are always options to decrease workload and increase motivation.
- Don’t be too hard on yourself; perfection does not exist. Do the best you can
- Take failures as opportunities for improvement.
- Work-life balance is important; there is a whole life outside the dental office.
- Practice Meditation /Mindfulness; they root you in the most important moment, the present.
- Practice Positive Psychology, look for at least three positive things in your daily life, and use a positive mindset to decompress your inner life.
Delivering high-quality dental care involves managing a range of cognitive and physical demands. The failure to address these factors can impair both the dentist’s performance and patient outcomes, potentially leading to burnout and complacency. Dentists should be trained on ergonomics and human factors principles from the early stages of education, and adopt strategies to manage workload, enhance team communication, invest in ergonomic equipment, and strive for a work-life balance. Combining these efforts fosters a safer, more efficient, and cognitively supportive environment where both patient and practitioner thrive.
- Cavalcante JL, Pinto AGA, Brito FE, Júnior, Moreira MRC, Lopes MVS, Rocha Cavalcante EG. Estresse ocupacional dos funcionários de uma universidade pública. Enferm Foco. 2019;10(4):108–15. Available from: http://dx.doi.org/10.21675/2357-707X.2019.v10.n4.2310
- Gupta A, Bhat M, Mohammed T, Bansal N, Gupta G. Ergonomics in dentistry. Int J Clin Pediatr Dent. 2014;7(1):30-4. Available from: https://doi.org/10.5005/jp-journals-10005-1229
- Marcum JA. An integrated model of clinical reasoning: dual-process theory of cognition and metacognition. J Eval Clin Pract. 2012;18:954–61. Available from: https://doi.org/10.1111/j.1365-2753.2012.01900.x
- Eva KW. What every teacher needs to know about clinical reasoning. Med Educ. 2005;39:98–106. Available from: https://doi.org/10.1111/j.1365-2929.2004.01972.x
- Scandurra C, Gasparro R, Dolce P, Bochicchio V, Muzii B, Sammartino G, et al. The role of cognitive and non-cognitive factors in dental anxiety: A mediation model. Eur J Oral Sci. 2021;129(4):e12793. Available from: https://doi.org/10.1111/eos.12793
- American Psychological Association. Psychologists, helping businesses and organizations. American Psychological Association. 2013. Available from: https://www.apa.org/education-career/guide/paths/business
- Grunberg NE, McManigle JE, Barry ES. Applying Classic Social Psychology Principles to Improve Healthcare Teams. MedEdPublish. 2021;9:251. Available from: https://doi.org/10.15694/mep.2020.000251.2
- Maake G. Assessment of motivational level in the workplace: Evidence from administrative employees. Int J Bus Ecosyst Strateg. 2024;6(3):106-16. Available from: https://doi.org/10.36096/ijbes.v6i3.497
- McDermott O, Antony J, Bhat S, Jayaraman R, Rosa A, Marolla G, et al. Lean Six Sigma in healthcare: A systematic literature review on motivations and benefits. Processes. 2022;10(10):1910. Available from: https://doi.org/10.3390/pr10101910
- Zhang M, Murphy B, Cabanilla A, Yidi C. Physical relaxation for occupational stress in healthcare workers: A systematic review and network meta-analysis of randomized controlled trials. J Occup Health. 2021;63(1):e12243. Available from: https://doi.org/10.1002/1348-9585.12243
- Harris K, Russ S. Patient-completed safety checklists as an empowerment tool for patient involvement in patient safety: concepts, considerations, and recommendations. Future Healthc J. 2021;8(3):e567-e573. Available from: https://doi.org/10.7861/fhj.2021-0122
- Marques-Sule E, Miró-Ferrer S, Muñoz-Gómez E, Bermejo-Fernández A, Juárez-Vela R, Gea-Caballero V, et al. Physical activity in healthcare professionals as a means of primary prevention of cardiovascular disease: A STROBE compliant cross-sectional study. Medicine (Baltimore). 2021;100(22):e26184. Available from: https://doi.org/10.1097/md.0000000000026184
- Schilbach M, Haun VC, Baethge A, Rigotti T. The challenging and hindering potential of time pressure: Qualitative job demands as suppressor variables. J Bus Psychol. 2023;38:1061–75. Available from: https://link.springer.com/article/10.1007/s10869-022-09844-w
- Rasool SF, Wang M, Tang M, Saeed A, Iqbal J. How toxic workplace environment affects employee engagement: The mediating role of organizational support and employee wellbeing. Int J Environ Res Public Health. 2021;18(5):2294. Available from: https://doi.org/10.3390/ijerph18052294
- Sjøgaard G, Lundberg U, Kadefors R. The role of muscle activity and mental load in the development of pain and degenerative processes at the muscle cell level during computer work. Eur J Appl Physiol. 2000;83(2-3):99-105. Available from: https://doi.org/10.1007/s004210000285
- Pronk NP, Martinson BC, Kessler RC, Beck AL, Simon GE, Wang P. The association between work performance and physical activity, cardiorespiratory fitness, and obesity. J Occup Environ Med. 2004;46(1):19-25. Available from: https://doi.org/10.1097/01.jom.0000105910.69449.b7
- Parry DA, Oeppen RS, Amin MSA, Brennan PA. Sleep: its importance and the effects of deprivation on surgeons and other healthcare professionals. Br J Oral Maxillofac Surg. 2018;56(8):663-666. Available from: https://doi.org/10.1016/j.bjoms.2018.08.001
- Plessas A, Nasser M, Hanoch Y, O'Brien T, Bernardes Delgado M, Moles D. Impact of time pressure on dentists' diagnostic performance. J Dent. 2019;82:38-44. Available from: https://doi.org/10.1016/j.jdent.2019.01.011
- Portoghese I, Galletta M, Coppola RC, Finco G, Campagna M. Burnout and workload among healthcare workers: the moderating role of job control. Saf Health Work. 2014;5(3):152-7. Available from: https://doi.org/10.1016/j.shaw.2014.05.004
- Langner R, Eickhoff SB. Sustaining attention to simple tasks: a meta-analytic review of the neural mechanisms of vigilant attention. Psychol Bull. 2013;139(4):870-900. Available from: https://doi.org/10.1037/a0030694
- Gawron V. Human Performance and Situation Awareness Measures. 3rd ed. CRC Press; 2019. Available from: https://doi.org/10.1201/9780429001024
- Bud M, Jitaru S, Lucaciu O, Korkut B, Dumitrascu-Timis L, Ionescu C, et al. The advantages of the dental operative microscope in restorative dentistry. Med Pharm Rep. 2021;94(1):22-27. Available from: https://doi.org/10.15386/mpr-1662
- Skinner A, Diller D, Kumar R, Cannon-Bowers J, Smith R, Tanaka A, et al. Development and application of a multi-modal task analysis to support intelligent tutoring of complex skills. Int J STEM Educ. 2018;5(1):14. Available from: https://doi.org/10.1186/s40594-018-0108-5
- Finkbeiner BL. Four-handed dentistry: instrument transfer. J Contemp Dent Pract. 2001;2(1):57-76. Available from: https://pubmed.ncbi.nlm.nih.gov/12167944/
- Kracher C, Breen C, McMahon K, Gagliardi L, Miyasaki C, Landsberg K, et al. The evolution of the dental assisting profession. J Dent Educ. 2017;81(9):eS30-eS37. Available from: https://doi.org/10.21815/jde.017.031
- U.S. Department of Labor, Occupational Safety and Health Administration (OSHA). Long Work Hours, Extended or Irregular Shifts, and Worker Fatigue. Available from: https://www.osha.gov/worker-fatigue/hazards
- World Health Organization (WHO). Burn-Out an “Occupational Phenomenon”: International Classification of Diseases. WHO; 2019. Available from: https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases
- Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397-422. Available from: https://doi.org/10.1146/annurev.psych.52.1.397
- Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377-85. Available from: https://doi.org/10.1001/archinternmed.2012.3199
- Afrashtehfar KI, Jurado CA. The dental profession experiences high prevalence rates of burnout and emotional exhaustion. J Evid Based Dent Pract. 2023;23(3):101886. Available from: https://doi.org/10.1016/j.jebdp.2023.101886
- Murthy VH. Confronting health worker burnout and well-being. N Engl J Med. 2022;387(7):577-579. Available from: https://doi.org/10.1056/nejmp2207252
- Razai MS, Majeed A. General practice in England: the current crisis, opportunities, and challenges. J Ambul Care Manag. 2022;45(2):135-139. Available from: https://doi.org/10.1097/jac.0000000000000410
- Waldo OA. The 3 “Rs” Relax, Reflect, and Regroup. Avoiding Burnout During Cardiology Fellowship. J Am Coll Cardiol. 2015;66(11). Available from: http://dx.doi.org/10.1016/j.jacc.2015.07.054